Partnership to Improve Postpartum Care In and Beyond the Neonatal Intensive Care Unit



Cooperative Agreement from the Centers for Disease Control and Prevention (CDC) to Advance Best Practices to Improve Postpartum Care In and Beyond the Neonatal Intensive Care Unit (“Care for NICU Families”)
Interdisciplinary Collaborative Receives $4 Million Cooperative Agreement from the CDC to Improve Postpartum Care In and Beyond the Neonatal Intensive Care Unit
New Funding Supports “Care for NICU Families” Research and Program
Chapel Hill, NC, October 2023 – The University of North Carolina at Chapel Hill’s Department of Pediatrics and Collaborative for Maternal and Infant Health, along with Reaching Our Sisters Everywhere, the University of California San Francisco’s (UCSF) School of Nursing and subject matter collaborative partners, have received a $4 million Cooperative Agreement from the Centers for Disease Control and Prevention (CDC) to Advance Best Practices to Improve Postpartum Care In and Beyond the Neonatal Intensive Care Unit (“Care for NICU Families”).
Collaborative partners include Mighty Little Giants, Breast Friends Lactation and Support Services, the 4th Trimester Project, Bellamy Management Consultants, Narrative Nation, the National Institute for Children’s Health Quality, the National Perinatal Association, Postpartum Support International, the Association of Women’s Health, Obstetric and Neonatal Nurses, Sabia Wade, and Heather Burris.

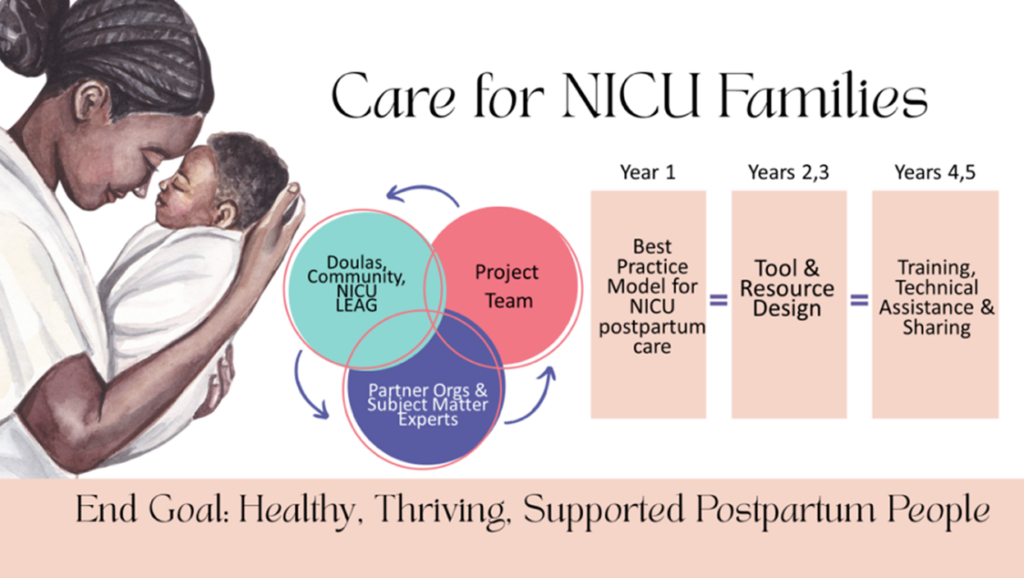
The team will build a national partnership guided by community and diverse lived experience voices to develop a set of Best Practices for Postpartum NICU Care along with co-created tools and strategies to support model care. They will share what they learn across NICUs, professional and community networks nationwide, and provide technical assistance to groups who are ready to make change. This will lead to increased awareness and use of effective data-informed clinical care and public health resources and interventions, as well as increased capacity to implement clinical and public health approaches to improve outcomes for postpartum people.
Co-Principal Investigator (Co-PI) Dr. Ifeyinwa Asiodu highlights that “The long-term goal of this important project is to eliminate perinatal health disparities and improve postpartum health and wellbeing during NICU stays through the transition to home. Continuity of care, including addressing the physical and mental health needs of the postpartum person and family, is critical to improving care for NICU families.“
The United States has one of the highest rates of maternal mortality and morbidity among wealthy countries (32.9 deaths per 100,000 birth) with unacceptable inequities due to historic and structural racism: Black birthing people experience a rate of maternal mortality 2.6 times higher than those who are White. “We know from previous research that mothers with infants in a NICU are more likely to have experienced a birth-related trauma, have depression/anxiety, lack access to basic care, have a chronic health condition, experienced a cesarean birth, and/or a blood transfusion, than mothers whose infants do not have a NICU stay,” Co-PI Dr. Sarah Verbiest underscored.
“NICUs are designed to address infant health, and they often do not accommodate the needs of postpartum people who are recovering from childbirth,” states Co-PI Dr. Wayne Price. NICU families describe challenges with basic practical needs, such as NICU visitor restrooms without menstrual products, going without meals to avoid leaving the infant’s bedside, and not taking pain medication / pulling over on the side of the road to sleep because there was no place to rest while visiting the NICU. He furthers, “Care for NICU Families” will increase awareness, resources, interventions, and capacity to make changes for NICU families on their postpartum journeys.”
Co-PI Dr. Kimarie Bugg concludes, “The “Care for NICU Families” team believes that better care for NICU postpartum parents will lead to improvements in outcomes for mothers and their babies by reducing maternal mortality and morbidity, increasing infant access to human milk, addressing maternal mental health and trauma, and providing NICU and community-based resources and social supports.”
You can learn more about the “Care for NICU Families” work at https://newmomhealth.com/about-care-for-nicu-families/.



About the UNC Collaborative for Maternal and Infant Health 4th Trimester Project, UNC Department of Pediatrics, UNC Jordan Institute for Families
The Collaborative for Maternal and Infant Health (UNC) team provides leadership on several state and national public health campaigns and quality improvement projects with experience in developing and implementing training and toolkits / evidence-based practice focused on systems to improve care for birthing people and their infants. They have implemented parent-designed tools for the American College of Obstetrics and Gynecology’s Postpartum Care Bundle and provide technical assistance to clinics across the country through the 4th Trimester Project (https://newmomhealth.com/healthcare).
The UNC team is housed within the UNC Departments of OB/GYN and Pediatrics which bring a wealth of clinical expertise. Dr. Verbiest also directs the Jordan Institute for Families at the UNC School of Social Work which focuses on building economic and social supports for families with young children.
NewMomHealth.com/about/our-team/ | www.MomBaby.org | JordanFamilies.org
About Reaching Our Sisters Everywhere
ROSE was founded to address breastfeeding disparities for communities of color. As a national expert and in partnership with communities across the country, they build equity in maternal and child health through culturally competent training, education, advocacy, and support.
About University of California San Francisco School of Nursing
University of California San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. Consistently ranked among the best nursing schools nationwide, the UCSF School of Nursing is a vibrant community of dedicated nurse leaders, nurse scientists, clinicians, students and staff who share a common drive to educate diverse health leaders, conduct research, advance nursing and provide public service that promotes health quality and equity. Learn more at nursing.ucsf.edu.
About The Centers for Disease Control and Prevention (CDC)
The Centers for Disease Control and Prevention (CDC) works to protect America’s health, safety, and security. The CDC uses grants and cooperative agreements to fund research and non-research public health programs that advance the agency’s public health mission domestically and abroad to keep Americans safe and healthy where they work, live, and play.
Media Contact: Suzanne Woodward, Communications Director, UNC Collaborative for Maternal and Infant Health (UNC CMIH), SuzanneW@med.unc.edu
Citations:
- Hoyert DL. Maternal mortality rates in the United States, 2021. NCHS Health E-Stats. 2023.
- Verbiest, S, Ferrari, R, Tucker, C, McClain, EK, Charles, N, Stub, AM (2020). “Health Needs of Mothers of Infants in a Neonatal Intensive Care Unit: A Mixed-Methods study.” Ann Intern Med 173(11_Supplement): S37-S44. And Stub, AM, Tucker, C, Ferrari, RM, McClain, E, onsson-Funk, M, Pate, V, Bryant K, Charles, N and Verbiest, S (2022). “Perinatal morbidity and health utilization among mothers of medically fragile infants.” J erinatol 42(2): 169-176.
- Ferrari, RM, McClain, EK, Tucker, C, Charles, N, Verbiest S, Lewis V, Bryant K, Stub AM (2022). “Postpartum Health Experiences of Women with Newborns in Intensive Care: The Desire to be by the e Infant Bedside as a Driver of Postpartum Health.” J Midwifery Women’s health.
To learn more about the “Care for NICU Families” Project and receive updates about this work, be sure you are subscribed to our listerv.
Explore Resources for NICU Parents from the 4th Trimester Project team. The team has also created free, open-access, evidence-based tools for care and community teams – Browse the Resource Center.
###
CARE For NICU Families. TM. 2023. Cooperative Agreement from the Centers for Disease Control and Prevention (CDC) to Advance Best Practices to Improve Postpartum Care In and Beyond the Neonatal Intensive Care Unit (“Care for NICU Families”)