Childbirth Trauma
Giving birth is a powerful experience and the journey often unfolds in ways we might not expect and cannot control.
Sometimes women feel that their transition to motherhood is traumatic. This may result from unexpected or unwanted medical interventions during labor and birth and/or postpartum, the speed at which they labored, the way that birth felt physically or emotionally, the ways in which they were treated, because of health complications for the mom or baby, or due to their deeply personal and unique experiences.
Those feelings are valid and true.
Women should be asked how they feel and listened to and supported by their healthcare team, family, friends, and others in their lives. This issue is not just about whether mom or baby are “ok” now – the ways we move through life matter too.
The World Health Organization offers guidance on respectful maternity care, which is centered around the concept of health as a human right. We all deserve to be treated with respect, dignity, and the highest quality care for our full selves. For those interested in being in community with others who experienced birth trauma, a Facebook Group called Traumatic Birth Stories and Support is available. It is described as“a safe place to talk honestly without judgment about what you have experienced, and to find the support of other moms who understand.”
Maternal Near-Miss
Maternal near-miss is a serious life event, in which a birthing person comes close to death due to a significant health problem.
The World Health Organization defines a maternal near-miss case as “a woman who nearly died but survived a complication that occurred during pregnancy, childbirth or within 42 days of the end of a pregnancy.” This is also sometimes called “severe maternal acute morbidity.” Although maternal deaths are relatively rare in the US (about 700 cases per year out of 4,000,000 deliveries), maternal near miss is more common. The Centers for Disease Control and Prevention estimates that there are around 50,000 cases in the US per year.
Examples of maternal near miss include but are not limited to postpartum hemorrhage (too much bleeding), heart attack, shock, kidney failure, or infection in the uterus. One or more body systems may be involved. Health care related to such complications can include maternal intensive care and, when indicated, response such as blood transfusion or hysterectomy (surgical removal of the uterus).
The physical complications of near miss may have lasting health impacts and so can the feelings related to what happened. Survival and the transition to motherhood with this mix of pain, grief, and new life is hard.
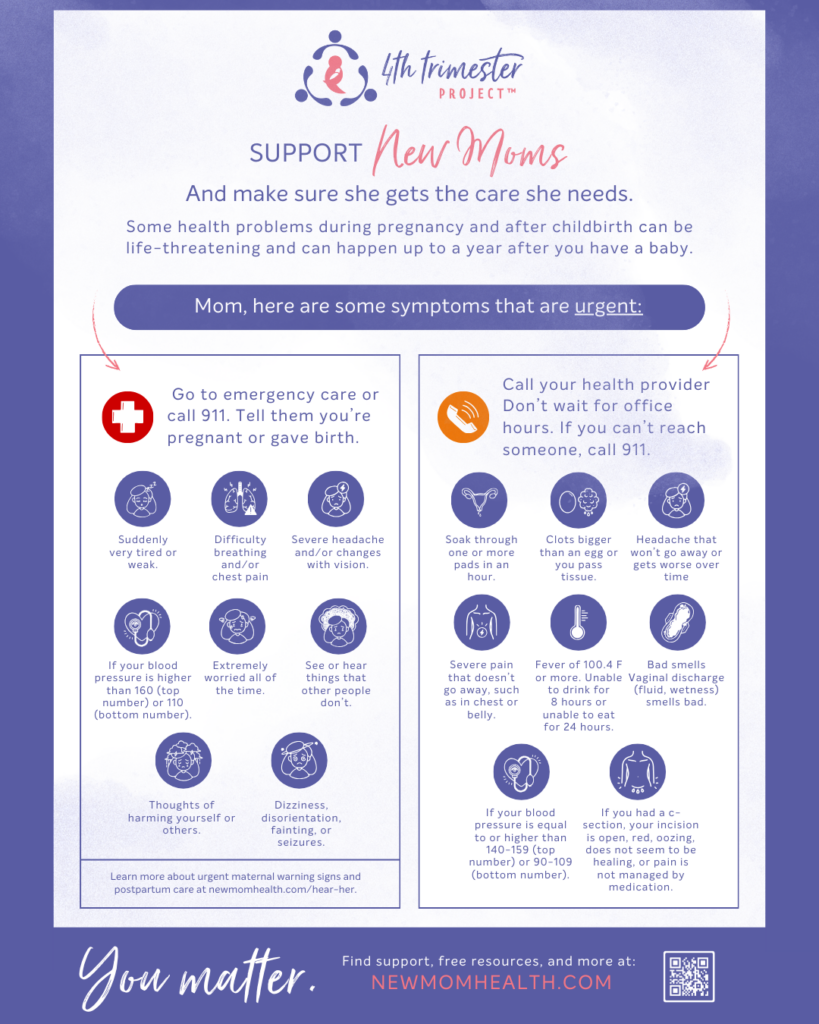
About 9% of women experience postpartum post-traumatic stress disorder (PTSD) following childbirth. Post-traumatic stress disorder (PTSD) typically happens after a traumatic or frightening childbirth experience, such as an emergency C-section, severe complications, or a scary threat to mom’s or baby’s life. Unexpected and scary medical situations can be hard to process and can interfere with bonding with baby. Know that this is treatable! Be sure to recognize the urgent maternal mental health warning signs, and what is considered a medical emergency.
The Maternal Near-Miss Survivors Facebook Group offers “a safe place where survivors find comfort and offer support as we journey toward healing together.”
Condition-specific resources:
Accreta/Increta/Percreta
- National Accreta Foundation: preventaccreta.org
Amniotic Fluid Embolism
- Amniotic Fluid Embolism Foundation: afesupport.org/get-support
Blood Clot
- National Blood Clot Alliance: www.stoptheclot.org
- Women & Blood Clots: womenandbloodclots.org/resources/
Heart Failure (pregnancy induced)
- Save the Mommies: https://savethemommies.com/
Postpartum Hemorrhage
- Life after postpartum hemorrhage: https://pqcnc-documents.s3.amazonaws.com/aim/PQCNCOBHPPHDischargeEd20180327.pdf
- March of Dimes: www.marchofdimes.org/pregnancy/postpartum-hemorrhage.aspx
Preeclampsia/Eclampsia/HELLP Syndrome
- EndPreeclampsia: www.endpreeclampsia.org
- Preeclampsia Foundation: www.preeclampsia.org/get-support
Sepsis
- Sepsis Alliance: https://www.sepsis.org/education/patients-family/faces-of-sepsis/?tag=pregnancy-childbirth
Mental health support:
- CDC Hear Her for New Families, Care Providers, and more – in multiple languages. View the Hear Her NC website page here
- New Parent Health One-Pager with details about warning signs
- View the Alliance for Innovation on Maternal Health resources
- Know there is anonymous, 24/7 support available. Learn about the maternal mental health hotline or call 1-833-9-HELP4MOMS
- Postpartum Support International has an online chat, resources, and PSI HelpLine: 1-800-944-4773 – #1 En Español or #2 English (Text in English: 800-944-4773 and Text en Español: 971-203-7773)
- Shades of Blue
- Maternal Mental Health Leadership Alliance Fact Sheets
- IRTH App for Black mothers