The pelvic floor is a group of muscles and tissues that stretch across the bottom of your pelvis. These muscles support your bladder, uterus, and anal/rectum. Your pelvic floors manages your bladder and bowel control, as well as sexual function.
During pregnancy and childbirth, your pelvic floor muscles can become weaker. Vaginal delivery can stretch and sometimes tear these muscles. Even cesarean deliveries can affect the pelvic floor due to the weight and pressure of the growing baby during pregnancy.
Common issues many moms face with their pelvic floor after childbirth include:
- Pelvic Floor Weakness: The muscles may become weak and can cause issues like urinary incontinence (leakage when you cough, sneeze, or laugh).
- Pelvic Organ Prolapse: This happens when the pelvic organs drop lower in the pelvis due to weakened support.
- Pain: Some women experience pain or discomfort in the pelvic region, making it hard to sit and walk comfortably.
Managing Pelvic Floor Health
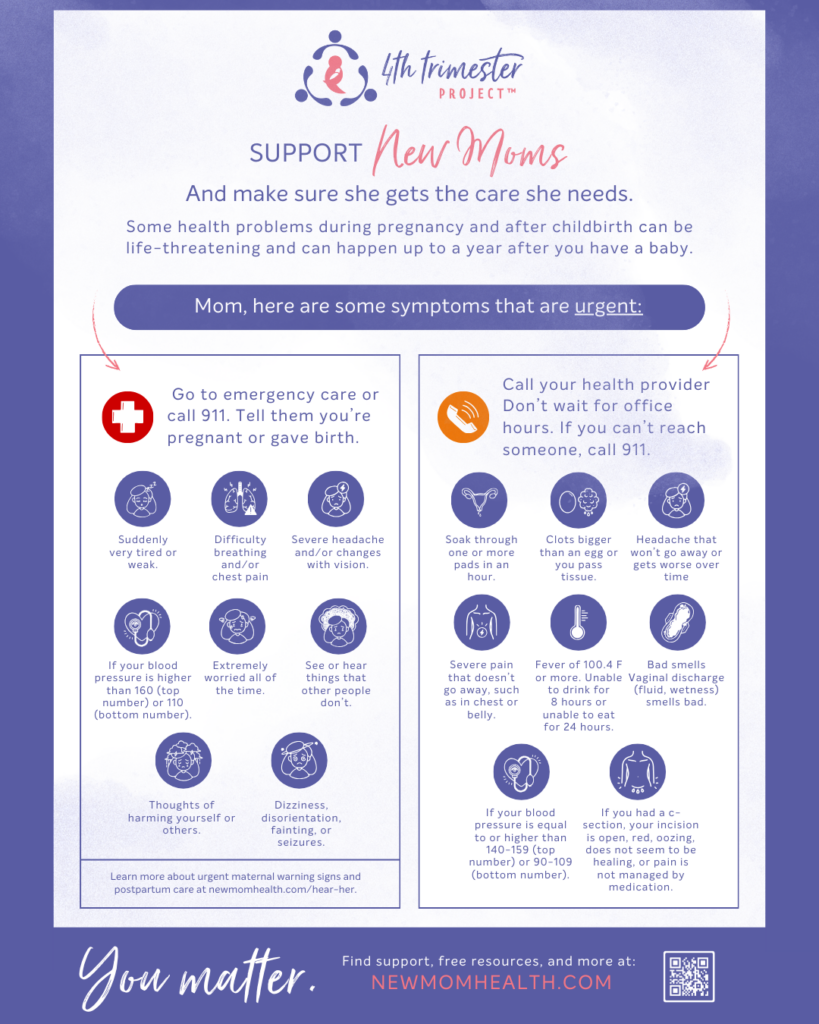
Postpartum Check-ups: Regular visits to your healthcare provider can help monitor your recovery. Normalize talking about any issues like incontinence or pain.
Physical Therapy: A pelvic floor physical therapist can provide personalized exercises and treatments to aid recovery. Many insurances now cover postpartum physical therapists.
Pelvic Floor Exercises: Kegels are an easy and free way to help strengthen the muscles in your vagina. Kegel exercises strengthen the muscles that are around the urethra, vagina, and anus. You can do them while at stoplights, during commercial breaks, while rocking your baby – anywhere! This is how the American College of Obstetricians and Gynecologists describes Kegels:
- With an empty bladder, squeeze muscles used to stop flow of urine
- Hold for 3 seconds, then relax for 3 seconds
- Do 10 series of Kegels at least three times a day
- Increase hold by 1 second each week up to 10 second holds
- Breath normally through these exercises
It can be confusing to know if Kegels are being done effectively. Your health care provider should be able to provide guidance, and potentially refer you to a pelvic floor therapist. If you want to keep your Kegels to yourself but still aren’t confident about how to do them, there are also app-based devices to guide you through biofeedback (like Elvie, Pericoach, Yarlap, KegelSmart, KGoal, Apex, Intensity). This pelvic floor exercise doesn’t solve everything, but may be a helpful start…unless your pelvic floor muscles are not only weak, but also tight.
If your pelvic floor muscles are too tight, you do NOT want to do Kegels, which just continue to contract your already over-contracted muscles. Instead, you want to figure out how to relax your pelvic floor, and strengthen it in the opposite way. All your muscles should have a full range of motion. Kegels help pelvic floors that are too weak to flex; they don’t help and can actually hurt pelvic floors that are too weak to unflex. Again, a physical or occupational therapist is probably your best bet. But there are also devices to help you self-diagnose (such as Renovia) and then choose exercises that are right for your body.
Stay Active: Gentle activities like walking or postpartum yoga can help maintain muscle tone and improve overall health.
Hydration and Diet: Drinking plenty of water and eating a high-fiber diet can prevent constipation, reducing strain on the pelvic floor.
Be Patient: Healing takes time. Be kind to your body and give yourself grace during this period of recovery.
Tight Pelvic Floor Muscle Symptoms
- Urinary symptoms
- Bladder pain
- Pain while urinating
- Frequent urination
- Difficulty starting or maintaining a urinary stream
- Bowel symptoms
- Difficulty starting a bowel movement (pooping)
- Feeling like you’re unable to empty completely
- Pain during or after pooping
- Pain with passing gas
- Constipation
- Sexual symptoms
- Pain during or after sex
- Inability to achieve orgasm
Resources to Explore:
- NAFC and this video
- National Association for Continence (NAFC) – Review of Three Pelvic Floor Exercise Devices.
- Also see My Care Team, where you can explore how a pelvic floor therapist might help
- Tight pelvic floor information