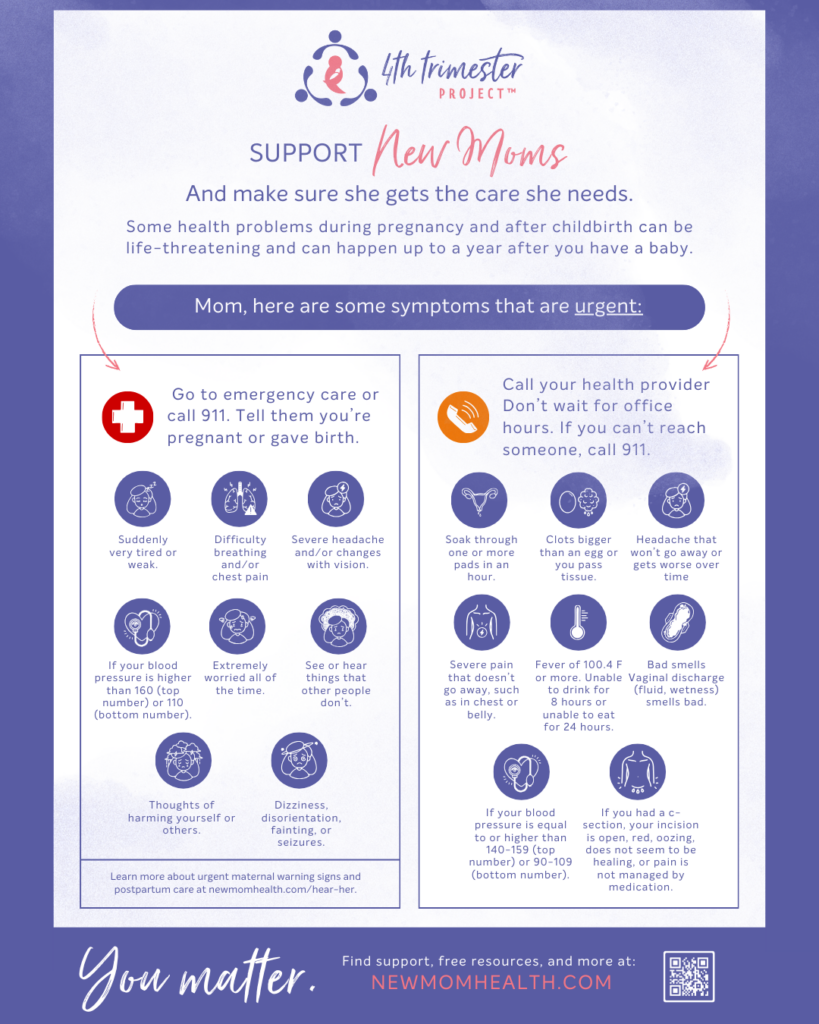
Did you know some health problems after giving birth are life-threatening and can happen up to a year after you have a baby? Support new moms and make sure they get the care they need.
Recognizing when something isn’t right and taking urgent action could save Mom’s life. Learn about and recognize the maternal health red flags, and what to do if you think you/someone has them.
Some maternal warning signs are physical – such as a temperate, blood pressure reading, headache, vision changes, stomach pain, and more. Some maternal health warning signs may not be visible, such as thoughts of harming a person, seeing things not there, overwhelming worry, sadness, or anxiety.
Print this one-page sheet on the urgent maternal health warning signs and symptoms. Stick it on your refrigerator or somewhere anyone who cares for mom can easily learn about and recognize the signs. Here is a brief training for family members/communities to know what to look for and what to do if a mother is experiencing warning signs.
What are the maternal health warning signs and what to do if you/someone is experiencing these:
You may be experiencing an emergency and should call 911 if you have any of these:
Tell them you’re pregnant or gave birth.
Changes in your body
- Suddenly very tired or weak.
- Difficulty breathing and/or chest pain
- Severe headache and/or changes with vision.
- Dizziness, disorientation, fainting, or seizures.
- If your blood pressure is higher than 160 (top number) or 110 (bottom number).
Feelings
- Extremely worried all of the time.*
- See or hear things that other people don’t.*
- Thoughts of harming yourself or others.*
- **In addition to calling 911, for mental health emergency support, be sure to call 988 (suicide hotline), and/or the maternal mental health hotline or PSI hotline – FREE, 24/7, anonymous in Eng/Spanish via text, chat, phone, and mobile app.
Make sure that you tell your health care team how long ago you gave birth.
Call your health care provider right away if you:
Don’t wait for office hours. If you can’t reach someone, call 911.
Bleeding
- Soak through one or more pads in an hour.
- Have clots bigger than an egg or you pass tissue.
Pain or swelling
- Headache that won’t go away or gets worse over time
- Severe pain that doesn’t go away, such as in chest or belly.
- Swelling, such as in face, hands, feet, or legs.
- If you had a c-section, your incision is open, red, oozing, does not seem to be healing, or pain is not managed by medication.
Changes in your body
- If your blood pressure is equal to or higher than 140-159 (top number) or 90-109 (bottom number).
- Fever of 100.4 F or more.
- Unable to drink for 8 hours or unable to eat for 24 hours.
Bad smells
- Vaginal discharge (fluid, wetness) smells bad.
Taking Care of You
Important postpartum health recovery information – to learn more or download a full resource, click here.
Feelings
- Trust your feelings and also get information and support. Caring for yourself is important.
- You matter and deserve to heal. Allow others to help and show they care.
Staying safe
- You should feel safe, physically and emotionally. If you do not feel safe, please speak with someone you trust and/or know. Anonymous support is available.
- Don’t drive when you are very tired or have difficulty focusing on the road.
Recovery
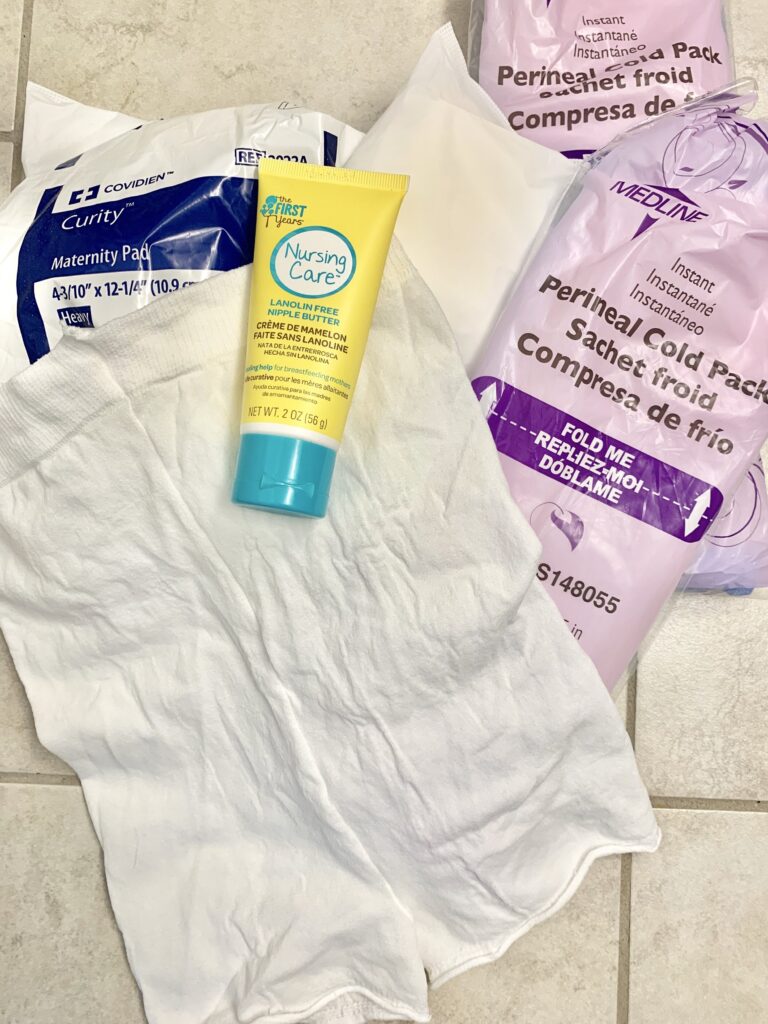
- Following birth, applying ice packs to your bottom can help with pain and reduce swelling. After a day or so, warm compresses, soaking your bottom area in warm water can feel good.
- Consider using a peri (squirt) bottle after using the toilet.
- Bleeding after birth (often called lochia) is normal. Quarter-sized blood clots are common the first few days.
- A number of nerves are cut during a cesarean section. It can take months for the incision area to feel normal.
Body changes
- Some people have varicose veins, stretch marks, extra skin, hair loss or different hair texture after giving birth. It can be hard to see your body change, but think of those as badges of honor.
- Incontinence is a common condition in which pee or poop comes out when you don’t want it to. Treatment is available and can help for pelvic floor problems.
Sex
- A lower sex drive after childbirth is common. Talk with your partner. If you are interested in having sex, consider using a lubricant.
- You are physically able to get pregnant a few weeks after childbirth. This is especially true if baby gets anything other than your milk.
- Talk to your provider about recovery, family planning goals, and your birth control options.
Breasts /chest
- Breast fullness and engorgement (when your breasts fill with milk and are firm to the touch) usually occurs around 3 to 7 days after delivery.
- Being in pain is stressful, and experiencing stress can make you feel more pain and cause breastfeeding problems. Get support right away.
Learn More: NewMomHealth.com > Self-Care
Maternal Health Warning Signs Resources:
We listen to mothers to determine the most important health information and also carefully recommend the organizations that we trust. The information here is not comprehensive nor is it medical advice; the content is intended to add to your health discussions and planning.
- Take and share this quick MHWS training for family members/communities to know what to look for and what to do if a mother is experiencing warning signs.
- CDC Hear Her for New Families, Care Providers, and more – in multiple languages. View the Hear Her NC website page here.
- New Parent Health One-Pager with details about warning signs
- Tips for Communicating with your health teams
- View the Alliance for Innovation on Maternal Health resources
- Know there is anonymous, 24/7 support available. Learn about the maternal mental health hotline or call 1-833-9-HELP4MOMS
- Download a one-page document about infant warning signs. Stick on your refrigerator to learn about emergencies and concerning symptoms.
- Postpartum Support International has an online chat, resources, and PSI HelpLine: 1-800-944-4773
#1 En Español or #2 English (Text in English: 800-944-4773 and Text en Español: 971-203-7773). - For those serving in the military: The Military Crisis Line, text-messaging service, and online chat provide free VA support for all Service members, including members of the National Guard and Reserve, and all Veterans, even if they are not registered with VA or enrolled in VA health care.